Keeping an eye on DNA-Based Vaccine
The science magazine “Scientific American” has recently included genetic vaccines in the “Ten technologies to keep an eye on”. The research of new vaccination strategies must take into consideration not only the vaccine-induced immune response, but also practical factors like ease of production, storage and costs: DNA meets most of these criteria, which makes it a suitable candidate for the generation of vaccines against infectious diseases or cancer.
This is the signal: there is an ongoing infection and the organism must react! As a result, a robust cytotoxic response is induced, where specialized immune effectors called CD8 T-lymphocytes release lytic enzymes that destroy infected cells. The same type of response is induced against a wide range of cancer proteins, which are synthetized in the cell cytoplasm starting from mutated or abnormally expressed DNA sequences and therefore different from healthy cells’ ones.
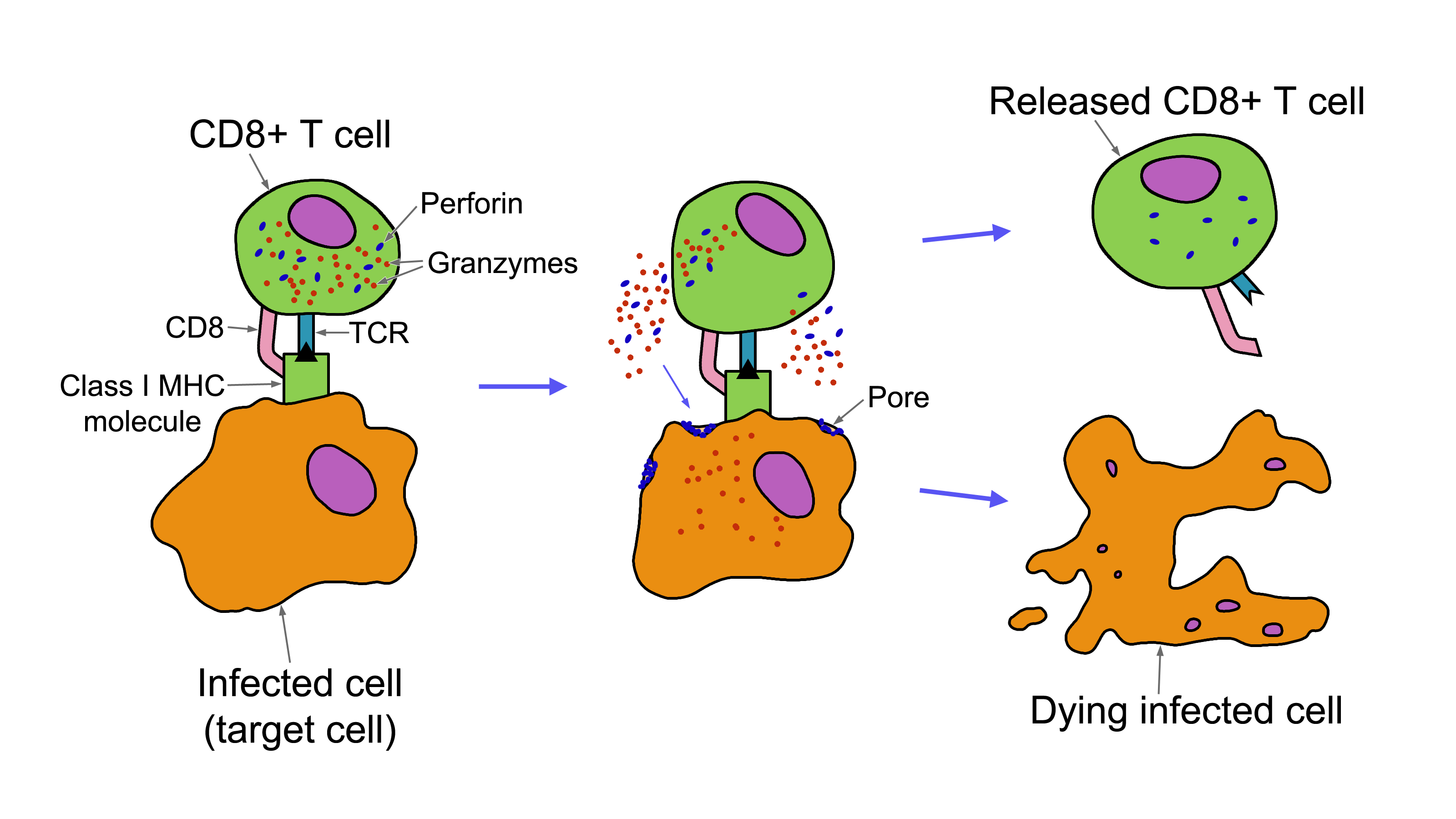
CD8 T lymphocytes recognize the “non-self” proteins exposed on the surface of infected cells through its T cell Receptor (TCR) and release lytic enzyme destroying them
There are also additional advantages, like ease of manipulation and large-scale production, costs and safety. In addition, a single vaccine can contain the genes coding for more proteins and be rapidly modified in the case of mutating pathogens or to include new features.
Nonetheless, the limitation with DNA is its poor intrinsic immunogenicity: most vaccines failed to induce significant immune responses in humans. This does not mean the end of DNA vaccines, but rather that we are still at the beginning! There is large room for improvement and researchers are at work to enhance DNA vaccine immunogenicity, studying new adjuvants, fusion with immunomodulatory sequences and delivery strategies.
Hopefully, we will continue to keep an eye on DNA vaccines while they make their way in medicine.
Erika Salvatori
Reference:
Geoffrey Ling (2017). Genomic Vaccines Fight Disease in Ways Not Possible Before. Scientific American.
This article is also available in Italian ![]()



